Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance
Related Articles: Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
- 1 Related Articles: Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance
- 2 Introduction
- 3 Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance
- 3.1 Demystifying the 60-Day Calendar: A Comprehensive Guide
- 3.2 The Importance of Understanding the 60-Day Calendar:
- 3.3 Frequently Asked Questions (FAQs) about the 60-Day Calendar:
- 3.4 Tips for Navigating the 60-Day Calendar:
- 3.5 Conclusion:
- 4 Closure
Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance
The Medicare program, a vital lifeline for millions of Americans aged 65 and over, offers a complex yet comprehensive system of healthcare coverage. Within this intricate framework lies a key element: the 60-day calendar. This calendar, often referred to as the "60-day rule," dictates the timing and duration of certain Medicare benefits, particularly those related to hospital stays and skilled nursing facility (SNF) care. Understanding this rule is crucial for beneficiaries to maximize their coverage and ensure seamless transitions between various healthcare settings.
Demystifying the 60-Day Calendar: A Comprehensive Guide
The 60-day calendar operates as a tracking mechanism for Medicare beneficiaries who require hospitalizations or SNF care. It essentially sets a time limit for these services, ensuring efficient utilization of resources and preventing unnecessary hospital stays.
Here’s how it works:
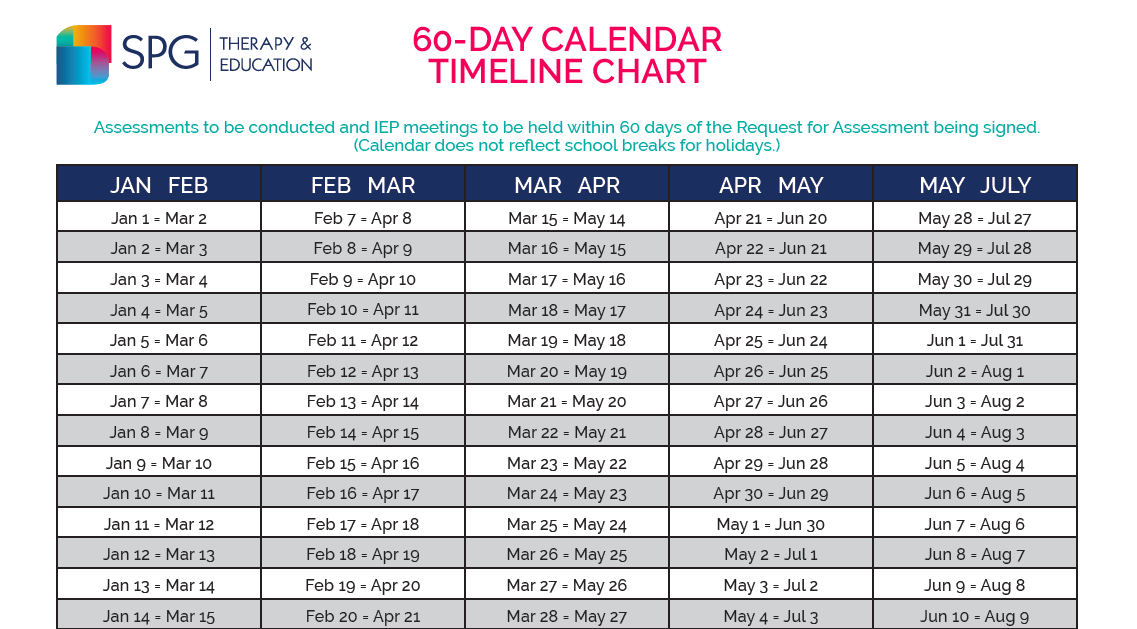
- Hospitalization: When a beneficiary is admitted to a hospital, the 60-day calendar begins ticking. The first 3 days of a hospital stay are considered a "benefit period." This means that Medicare will cover the majority of the costs for these initial days.
- Skilled Nursing Facility (SNF) Care: If a beneficiary requires skilled nursing care after a hospital stay, they may be eligible for SNF coverage. However, this coverage is contingent on the hospital stay meeting certain conditions, including a minimum stay of 3 days. The 60-day calendar plays a critical role here.
-
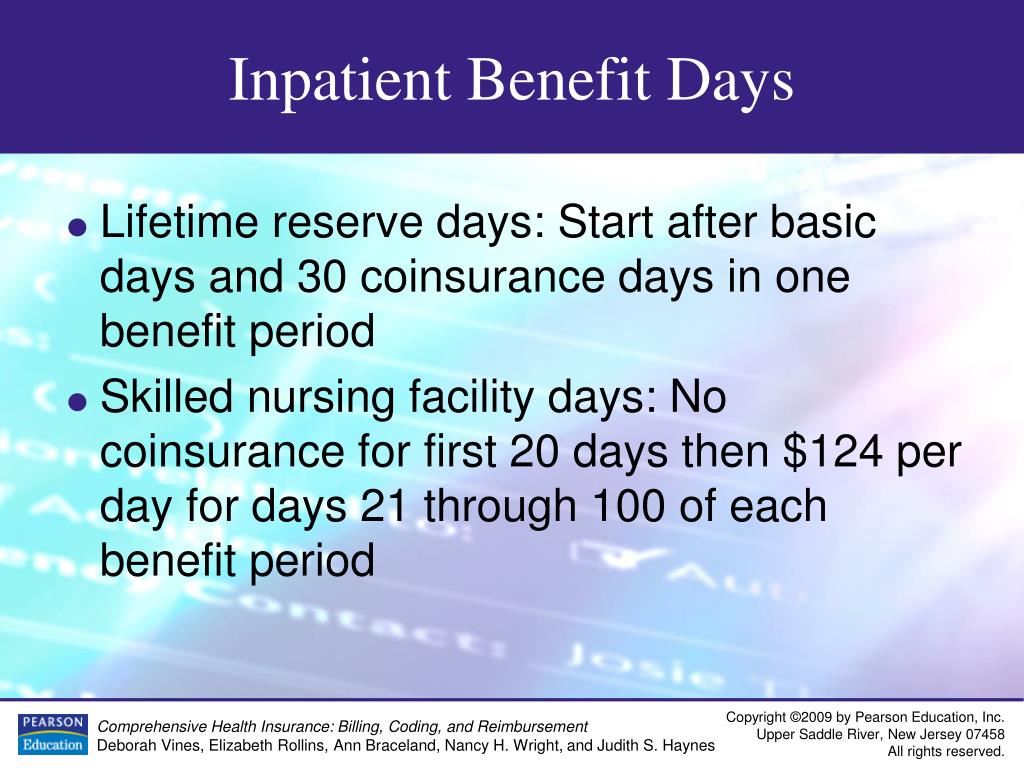
60-Day Limit: Medicare generally covers up to 100 days of SNF care within a single benefit period. However, this coverage is split into two segments:
- First 20 Days: Medicare covers all costs for the first 20 days of SNF care.
- Days 21-100: Beneficiaries are responsible for a daily co-payment for days 21 through 100.
- New Benefit Period: After the 100-day limit is reached, a new benefit period begins. This means that the beneficiary can once again receive 100 days of SNF coverage, provided they meet the hospital stay requirements.
Crucial Considerations:
- Benefit Period: Each hospital stay initiates a new benefit period. This means that if a beneficiary has a second hospital stay within the same calendar year, they can receive another 100 days of SNF coverage.
- Lifetime Reserve Days: Medicare also offers a "lifetime reserve" of 60 days. These days can be used if a beneficiary exhausts their 100-day benefit period within a single calendar year. However, these days are non-renewable and can only be used once in a lifetime.
- Medicare Part A: The 60-day calendar is primarily governed by Medicare Part A, which covers hospital stays and SNF care. Medicare Part B, which covers outpatient services, does not directly utilize this calendar.
The Importance of Understanding the 60-Day Calendar:
Navigating the Medicare system can be daunting, and the 60-day calendar adds another layer of complexity. However, understanding this rule is crucial for beneficiaries to:
- Ensure Timely Access to Care: By understanding the 60-day calendar, beneficiaries can proactively plan for their healthcare needs, ensuring they have access to necessary services when needed.
- Maximize Coverage: Knowing the limitations of the 60-day calendar allows beneficiaries to make informed decisions about their care, ensuring they receive the maximum coverage available to them.
- Avoid Unnecessary Expenses: Being aware of the co-payment structure for SNF care beyond the first 20 days can help beneficiaries budget for potential expenses.
- Optimize Transitions: The 60-day calendar provides a framework for smooth transitions between hospital and SNF care, minimizing the risk of unnecessary delays or disruptions in care.
Frequently Asked Questions (FAQs) about the 60-Day Calendar:
1. What happens if I use up my 100 days of SNF care within a calendar year?
If you exhaust your 100 days of SNF coverage within a calendar year, you can utilize your lifetime reserve days. This provides you with an additional 60 days of coverage. However, these days are non-renewable and can only be used once in your lifetime.
2. Do I need to be hospitalized for 3 days to qualify for SNF care?
Yes, you need to have been hospitalized for at least 3 consecutive days for a qualifying condition to be eligible for SNF coverage. This 3-day stay initiates a new benefit period.
3. How do I know how many days of SNF coverage I have left?
You can contact your Medicare provider or visit the Medicare website to access your personal coverage information. This will show you your remaining SNF coverage days.
4. What if I need SNF care after my 100 days are used up?
If you require skilled nursing care after exhausting your 100-day benefit period, you will need to pay for the care out-of-pocket, unless you have private insurance or other coverage.
5. How do I know if my hospital stay qualifies for SNF coverage?
Your doctor will determine if your hospital stay meets the criteria for SNF coverage. They will also discuss your care plan and assess your need for skilled nursing services.
6. Can I use my 60-day calendar for multiple hospital stays?
Yes, each hospital stay initiates a new benefit period, allowing you to receive 100 days of SNF coverage again.
7. What are the co-payments for SNF care after the first 20 days?
The co-payment for days 21-100 of SNF care varies depending on your specific Medicare plan. You can contact your provider or visit the Medicare website for detailed information.
8. Can I choose to use my lifetime reserve days even if I haven’t used up my 100 days?
No, you can only use your lifetime reserve days once you have exhausted your 100-day benefit period within a calendar year.
9. What if I am hospitalized for a short period?
Even a short hospital stay can trigger a new benefit period. If you need SNF care after a short hospital stay, you will be eligible for the full 100 days of coverage.
10. What if I have a chronic condition that requires ongoing SNF care?
If you have a chronic condition that requires ongoing SNF care, you may need to explore alternative options, such as home health services, to ensure you receive the necessary care.
Tips for Navigating the 60-Day Calendar:
- Stay Informed: Familiarize yourself with the 60-day calendar rules and your specific Medicare coverage.
- Communicate with Your Doctor: Discuss your healthcare needs and potential SNF care requirements with your doctor.
- Plan Ahead: If you anticipate needing SNF care, plan your hospital stays and potential SNF admission dates.
- Keep Records: Maintain records of your hospital stays and SNF care to track your coverage days.
- Seek Assistance: Don’t hesitate to reach out to your Medicare provider or a Medicare counselor for help navigating the system.
Conclusion:
The 60-day calendar is an integral component of the Medicare system, ensuring efficient utilization of resources and providing a framework for managing hospital and SNF care. By understanding the rules and limitations of this calendar, beneficiaries can make informed decisions about their healthcare needs, maximize their coverage, and avoid unnecessary expenses. Staying informed and proactive is key to navigating the complex Medicare landscape and ensuring you receive the best possible care.


![Navigating Medicare [INFOGRAPHIC]](https://www.thenoblegroup.com/-/media/rj/common/resources/retirement/navigating-medicare-2023-1.png)

+calendar+%26+chart.png)
Closure
Thus, we hope this article has provided valuable insights into Navigating the Medicare Landscape: Understanding the 60-Day Calendar and Its Significance. We appreciate your attention to our article. See you in our next article!